Digital Twins in Healthcare: Revolutionizing Patient Care at Duke

Digital twin technology is transforming industries by creating precise virtual replicas of physical systems—and I’ve seen how its application in healthcare can revolutionize patient care.
At the Duke Center for Computational and Digital Health Innovation, our interdisciplinary teams are pioneering this advanced technology, combining engineering, medicine, and advanced computing to address critical challenges in healthcare. By using digital twins, we’re advancing personalized treatments, optimizing surgical planning, and improving long-term health outcomes.
What are digital twins?
Digital twins are virtual models that replicate real-world objects or systems. In healthcare, digital twins can be virtual representations of organs, such as the heart or lungs, entire physiological systems, or even a patient’s full body.
Unlike static computational models, digital twins dynamically integrate real-time data, such as from wearable sensors, to reflect the unique characteristics of a person. This ensures that the model is not just a generalized representation, but a personalized tool tied directly to the patient’s specific health profile.
By creating digital replicas of patient-specific anatomy, we can diagnose, treat, and even predict disease progression with unprecedented accuracy.
This shift from reactive to proactive care represents a major leap forward. For example, imagine diagnosing heart conditions and creating an optimal treatment plan without invasive procedures. That’s what we make possible by creating personalized digital twins of each patient’s blood flow.
Building a digital twin: a collaborative process
Digital twin technology thrives on collaboration between fields like engineering, AI, and medicine.
The process typically begins by defining the physical object or system to be replicated. Data is then collected from various sources, such as imaging technologies, EHRs, and wearable devices, to construct a detailed virtual model.
This virtual model is dynamic, meaning it continuously updates with real-time data transmitted through IoT devices and other sensors. Advanced analytics, machine learning, and simulation tools are employed to analyze this data, predict future scenarios, and optimize outcomes.
Validation is critical: The model must accurately mirror the physical system and adjust as new information becomes available. Finally, a feedback loop ensures that insights derived from the digital twin can be acted upon in real-world clinical settings, whether to refine treatments, improve operational workflows, or predict patient outcomes.
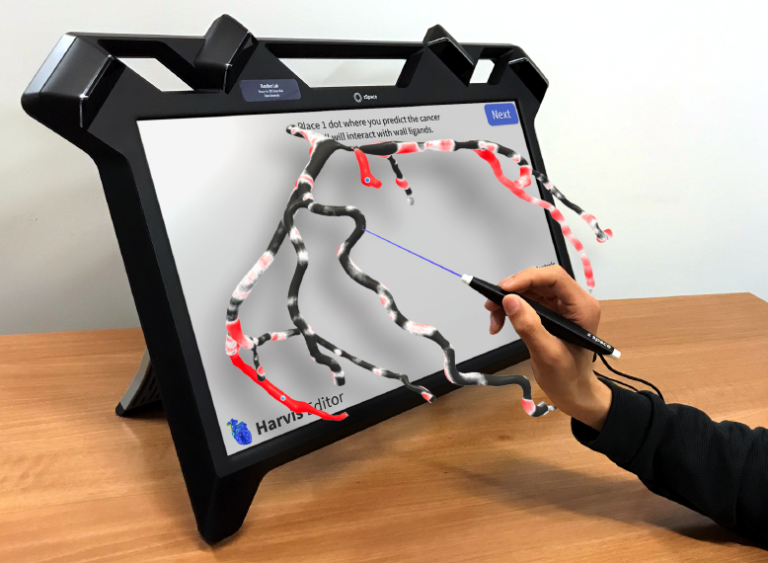
In my lab, our focus is on creating digital twins to diagnose and treat conditions such as cancer and heart or carotid disease. Our process begins with image segmentation, where advanced AI tools isolate specific regions of a patient’s vasculature.
The next step is 3D reconstruction. We create detailed models of a patient’s vascular structure, which can be very complex. Accurate segmentation requires extracting these intricate anatomies from MRI and CT scans—an often difficult and time-consuming process.
Finally, simulation integrates hospital data, such as blood flow characteristics, to create realistic models. This step enables clinicians to simulate various scenarios, compare treatment options, and anticipate patient outcomes.
Digital twin applications in healthcare
The Center’s multidisciplinary research teams use digital twin technology to tackle various conditions spanning cardiology, neurology, and peripheral arterial disease. Our researchers are exploring diverse applications of this technology, such as:
Proactive monitoring
Wearables combined with digital twins enable real-time health monitoring. This approach shifts healthcare from reactive to proactive, addressing issues before they escalate. By continuously collecting and analyzing data such as heart rate, blood pressure, and activity levels, wearables provide an ongoing stream of information that digital twins use to model a patient’s evolving health.
Surgical planning
Using digital twins, surgeons can simulate procedures in a virtual environment before operating on a patient. We’re working with David Hasan, M.D., to develop vascular digital twins so that procedures can be simulated before performing them on patients. This is exciting because it would allow physicians to practice interventions like stent placement—determining the size and placement—and potentially minimize complications associated with the procedure.
Long-term outcome prediction
Digital twins allow physicians to simulate the long-term effects of interventions, compressing time to predict how conditions might evolve over the years. For patients with vascular diseases, for example, it can enable earlier interventions to prevent complications and improve outcomes.
Benefits and challenges of digital twins in healthcare
My colleague Manesh Patel, M.D., chief of the Duke Division of Cardiology, often points out that the advantages of digital twins are numerous. Not only are they patient-specific, but they allow doctors to compare different interventions before that patient even makes it to the operating room.
Indeed, digital twins’ capacity for personalization is revolutionary. Unlike traditional diagnostic tools, they create a highly individualized representation of a patient’s anatomy and physiology. By tailoring simulations to the unique characteristics of each patient, they provide insights that are often impossible to obtain through one-size-fits-all approaches.
Another significant benefit is their role in enabling proactive care. When paired with wearables and other real-time monitoring devices, digital twins allow clinicians to detect potential health issues before symptoms appear or conditions worsen. This early detection translates to reduced healthcare costs by preventing complications and minimizing hospital stays.
Digital twins also assist in decision-making by empowering clinicians to simulate and evaluate multiple scenarios in a risk-free environment. For example, a surgeon can use a digital twin to model different approaches to a procedure, identifying the strategy most likely to result in success. This ability is particularly valuable in complex cases where uncertainty can lead to suboptimal outcomes.
But implementing digital twins in healthcare also comes with challenges. Managing and utilizing the vast amounts of data required for these models is a daunting task. Consider that of all the data on Earth, it’s estimated that 30 percent is health data. Every year, hospitals generate around 50 petabytes of data—yet 97 percent of that’s not used to improve anyone’s health.
As Dr. Patel says, one thing he can guarantee is that there will be more and more data available in the coming years. Robust data management systems and tools are needed to extract meaningful insights from the sea of information.
Additionally, integrating wearables and computational models into everyday clinical workflows demands seamless collaboration between technologists and healthcare providers, as well as significant investments in infrastructure and training.
Duke’s leadership in digital twins
As digital twins continue to develop, the coming years promise significant advancements that could redefine healthcare. Experts predict the technology will see exponential growth, becoming a multibillion-dollar industry by 2027.
By investing in interdisciplinary research and leveraging advanced computing, Duke is shaping the future of healthcare. Learn more about collaborating with us to drive progress in computational health innovation.
Amanda Randles, Ph.D., is Director of the Duke Center for Computational and Digital Health Innovation and Alfred Winborne Mordecai and Victoria Stover Mordecai Associate Professor of Biomedical Engineering at the Pratt School of Engineering.