Analysis identifying minimal governing parameters for clinically accurate in silico fractional flow reserve
Frontiers in Medical Technology
Cyrus Tanade, S. James Chen, Jane A. Leopold, and Amanda Randles
Summary
Personalized hemodynamic models can accurately compute fractional flow reserve (FFR) from coronary angiograms and clinical measurements (FFRbaseline), but obtaining patient-specific data could be challenging and sometimes not feasible. Understanding which measurements need to be patient-tuned vs. patient-generalized would inform models with minimal inputs that could expedite data collection and simulation pipelines.
Our aims were to determine the minimum set of patient-specific inputs to compute FFR using invasive measurement of FFR (FFRinvasive) as gold standard.
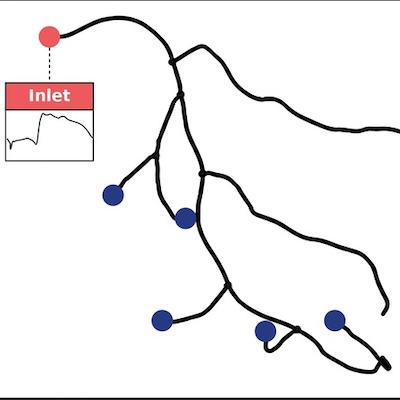
Personalized coronary geometries (N=50) were derived from patient coronary angiograms. A computational fluid dynamics framework, FFRbaseline, was parameterized with patient-specific inputs: coronary geometry, stenosis geometry, mean arterial pressure, cardiac output, heart rate, hematocrit, and distal pressure location. FFRbaseline was validated against FFRinvasive and used as the baseline to elucidate the impact of uncertainty on personalized inputs through global uncertainty analysis. FFRstreamlined was created by only incorporating the most sensitive inputs and FFRsemi-streamlined additionally included patient-specific distal location.
FFRbaseline was validated against FFRinvasive via correlation (r=0.714, p<0.001), agreement (mean difference: 0.01±0.09), and diagnostic performance (sensitivity: 89.5%, specificity: 93.6%, PPV: 89.5%, NPV: 93.6%, AUC: 0.95). FFRsemi-streamlined provided identical diagnostic performance with FFRbaseline. Compared to FFRbaseline vs. FFRinvasive, FFRstreamlined vs. FFRinvasive had decreased correlation (r=0.64, p<0.001), improved agreement (mean difference: 0.01±0.08), and comparable diagnostic performance (sensitivity: 79.0%, specificity: 90.3%, PPV: 83.3%, NPV: 87.5%, AUC: 0.90).
Streamlined models could match the diagnostic performance of the baseline with a full gamut of patient-specific measurements. Capturing coronary hemodynamics depended most on accurate geometry reconstruction and cardiac output measurement.
Citation
Tanade, Cyrus, et al. “Analysis identifying minimal governing parameters for clinically accurate in silico fractional flow reserve.” Frontiers in Medical Technology 4 (2022): 1034801.