Wearables
Wearable technology and biosensors represent a groundbreaking stride in health monitoring, offering continuous, real-time data that was once unattainable. The integration of wearable technology into health research and care signifies a pivotal shift toward proactive and preventive health management.
At the Duke Center for Computational and Digital Health Innovation, wearable sensors form a cornerstone of our mission to revolutionize healthcare. These sensors, combined with advanced machine learning, enable us to monitor patient activity in real time, providing unprecedented insights into health and wellness.
What Are Wearable Sensors?
Wearable sensors are compact, body-worn devices designed to continuously collect data on a plethora of vital information as individuals engage in their daily activities, enabling a nuanced and dynamic picture of their health status. Wearables include fitness trackers and smartwatches as well as specialized medical devices
By analyzing the vast amounts of information gathered by wearables, researchers and clinicians can identify patterns, predict health trends, and tailor interventions in a timely and more personalized manner.
Types of Data We Collect with Wearable Sensors
Through wearable sensors, we gather a wide array of data, including:
- Physical activity: Step counts, movement patterns, and activity levels
- Vital signs: Heart rate, respiratory rate, and oxygen saturation
- Behavioral data: Sleep patterns and energy expenditure
- Biometric trends: Temperature, hydration levels, and emerging biomarkers
How We Use Data from Wearable Sensors
At the Center for Computational and Digital Health Innovation, we harness the power of wearable technology to propel our understanding and management of human health to unprecedented levels.
Proactive Health Management
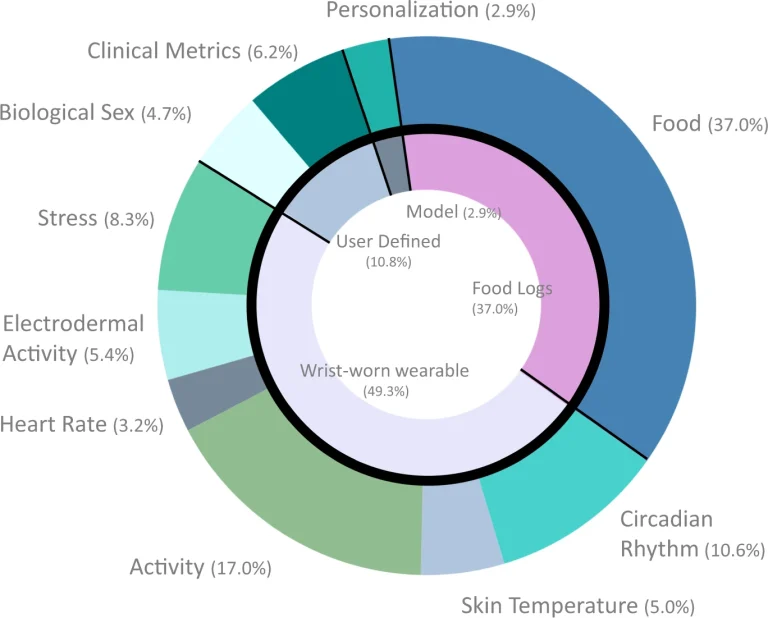
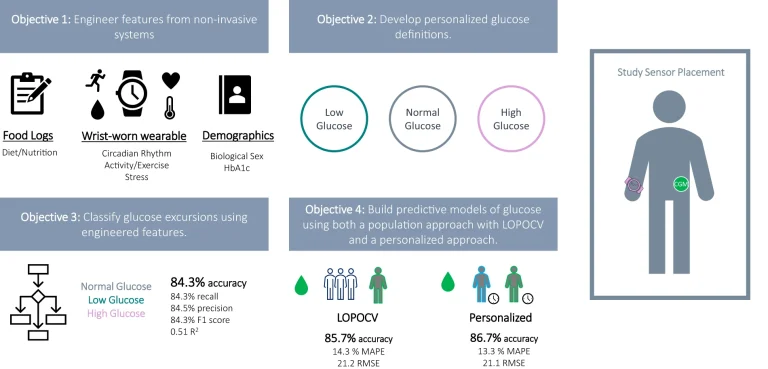
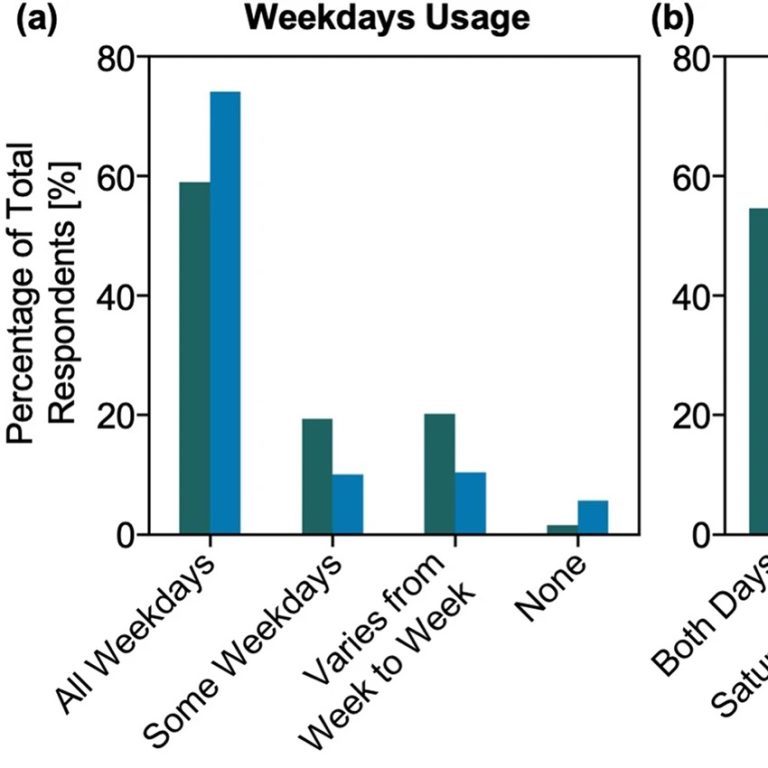
The BIG IDEAs Lab led by Dr. Jessilyn Dunn is dedicated to integrating technology and population health approaches to empower proactive health management. By using wearables, the lab captures vital health metrics such as heart rate, activity levels, and sleep patterns in real-world settings.
The continuous stream of data allows the development of computational tools and machine learning algorithms that process and interpret information in real time. This enables early detection of health issues and the creation of personalized interventions, shifting the approach to healthcare from reactive to proactive.
Developing new care delivery models
The Health Innovation Lab, led by Dr. Ryan Shaw, focuses on integrating patient-generated health data into new care delivery models. The lab uses wearables, sensors, and other emerging health technologies to enhance patient care, particularly for managing chronic conditions like diabetes and hypertension.
The research emphasizes health equity, ensuring that these technologies benefit a diverse patient population, including those from underserved communities. The lab has demonstrated that data from wearables can be integrated into electronic health records, supporting innovative care models that are both clinically effective and financially sustainable.

Jessilyn Dunn with PhD student Brinnae Bent who is preparing to download information from a wearable health monitoring device
Monitoring physiological response

In the field of anesthesiology, Dr. Leah Acker’s research utilizes wearables to monitor patients’ physiological responses, particularly during and after surgery. By collecting continuous data on parameters such as heart rate and blood pressure, wearables help identify potential complications early and guide timely interventions. This approach enhances patient safety and improves outcomes by providing clinicians with real-time insights into patients’ conditions.
Monitoring patient-specific hemodynamics over time
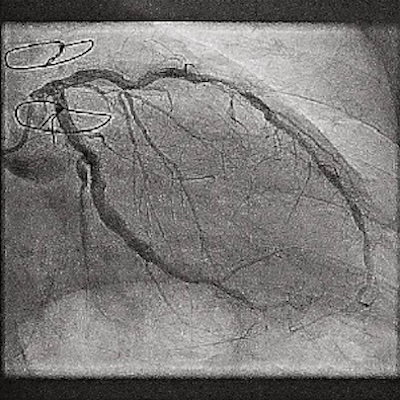
The Randles Lab focuses on high-fidelity and personalized hemodynamic simulations, particularly in cardiovascular research. By collecting patient-specific data from wearables, the lab creates digital twins to simulate blood flow and disease progression over time. This effort is exemplified by the Longitudinal Hemodynamic Mapping framework, which enables detailed tracking of blood flow dynamics and disease progression across millions of heartbeats.
These models allow for detailed analysis of how changes in physiological states, captured by wearables, influence blood flow dynamics. This research has strong potential for understanding and predicting conditions like coronary artery disease, offering clinicians valuable tools for early intervention and personalized treatment strategies.