Wearables in Action: Transforming Patient Care Through Proactive Health Monitoring

Wearables are revolutionizing modern healthcare monitoring.
No longer simply flashy consumer gadgets, they’re rapidly becoming indispensable clinical tools, helping us identify at-risk patients sooner and customize treatments more accurately. Physicians have long relied on periodic visits to capture patients’ vital health information, but with wearables, they can now access a steady flow of metrics — heart rate, activity levels, and more — in real time.
This constant feedback loop allows for earlier detection of subtle changes, leading to more targeted interventions and better overall outcomes. By gathering data in daily-life settings, wearables also capture a truer picture of health — one that transcends the artificial confines of an exam room.
The immense potential of wearables is clear: Armed with continuous, real-world data, healthcare can shift from reacting to crises to preventing them.
At the Duke Center for Computational and Digital Health Innovation, my colleagues and I are exploring how wearables will redefine healthcare, making continuous monitoring the new standard.
What are wearables?
Wearables are smart devices designed to be worn on the body, continuously collecting and transmitting physiological data. They include:
- Smartwatches
- Fitness trackers
- Biometric clothing
- Smart contact lenses
- Implanted sensors
They can monitor a variety of health metrics, including heart rate, blood pressure, oxygen levels, temperature, and activity levels. Some advanced models are equipped with ECG sensors, glucose monitors, and motion detectors that can help assess conditions like arrhythmias, diabetes, and fall risks.
Wearables can be categorized based on their function and design. Some are external, like wristbands and smart patches, while others are embedded within the body to track internal conditions. For example, smart textiles and bio-integrated sensors can measure hydration levels or skin conductivity or even detect early signs of infection.
Over the past decade, consumer adoption of wearables has surged, with many people using them to take a more active role in their health. These devices can reinforce positive habits, increase self-awareness, and even integrate with behavioral counseling for greater impact.
And now they’re expanding beyond consumer tech, fundamentally redefining modern healthcare.
How wearables work to ‘Find, Track, Treat’
Wearables play a key role in our mission to identify, monitor, and treat health issues in a proactive, personalized manner.
By continuously collecting data — like heart rate variability or subtle changes in gait — these devices help us find early warning signs long before symptoms become obvious. For instance, arrhythmias that might go undetected in a typical exam can surface through weeks of real-world heart rhythm data.
Once a condition is flagged, ongoing monitoring allows our teams to track disease progression. AI algorithms pick up slight deviations from a patient’s normal patterns, enabling clinicians to react promptly — whether that means adjusting medication or scheduling an extra check-up.
Finally, in the treat phase, real-time insights help tailor interventions for each patient, from specialized rehab exercises to refinements in surgical planning. The result is higher adherence, fewer complications, and better patient outcomes.
My Duke colleagues and I are exploring different dimensions of wearable research:
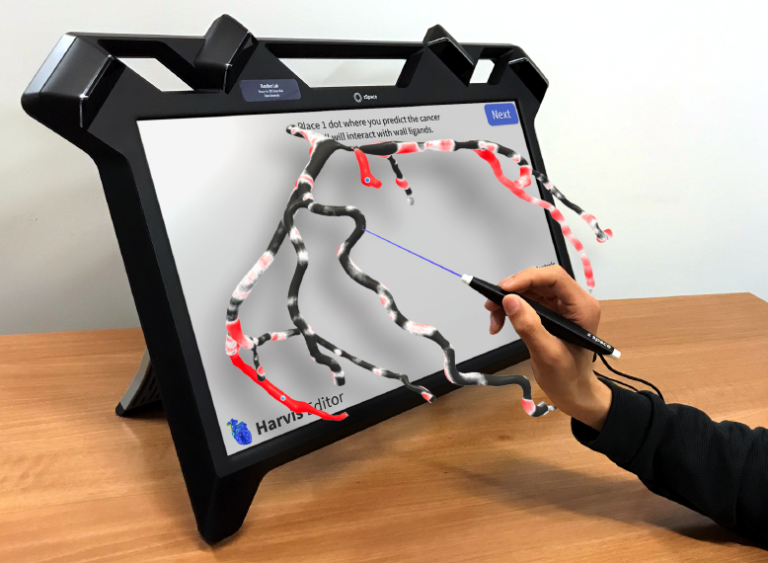
- My lab, the Randles Lab, employs wearable-derived metrics to power digital twins that can detect subtle blood flow anomalies and provide cardiologists and surgeons with clearer insights for clinical decision-making. By continuously integrating real-world data, these models allow clinicians to track changes in blood flow over time, potentially detecting complications like in-stent restenosis before symptoms appear.
- The BIG IDEAs Lab, led by Dr. Jessilyn Dunn, focuses on real-time population health. Wearable sensors gather raw data on factors like heart rate and sleep quality, and machine learning transforms these into actionable indicators for disease prevention and personalized health optimization. This platform also creates valuable opportunities for industry collaborators to refine algorithms and device design.
- The School of Nursing’s Health Innovation Lab, led by Dr. Ryan Shaw, integrates patient-generated data directly into care models. By testing devices in simulated clinical environments, they ensure solutions are ready for broader adoption, which is made even more feasible by new reimbursement pathways for integrating wearable technology into clinical practice.
- The ACkER Lab, led by Dr. Leah Acker, monitors older adults before, during, and after surgery, using continuous sensors to pinpoint why some patients bounce back quickly while others struggle. These large-scale data sets also invite research partnerships to build better predictive models.
Together, these projects demonstrate the vast potential of wearables to reshape how we diagnose, monitor, and treat disease.
Overcoming challenges and ensuring impact
Integrating wearable data into clinical workflows calls for close collaboration among engineers, data scientists, and healthcare providers — something we do particularly well at Duke. We understand that while wearables offer transformative potential, they also introduce significant challenges that must be addressed collaboratively.
We invest in informatics platforms that securely sync sensor readings with electronic health records so that clinicians can get actionable insights when they need them most. At the same time, interoperability remains a hurdle, as different devices generate vast amounts of data that must be standardized and integrated into existing healthcare systems.
We also understand the pressing need to address privacy concerns, ethical standards, and potential algorithmic biases — especially as large-scale datasets can inadvertently overlook certain populations.
Scalability and accessibility matter just as much. Wearables are becoming more affordable and user-friendly, but disparities in digital literacy and access to reliable internet connections could limit their impact for some patients. Partnerships with device manufacturers or support from philanthropic and governmental organizations can help lower costs, improve usability, and extend wearable adoption, particularly for underserved communities.
Future innovations in wearable tech
Wearables and artificial intelligence are fast reshaping how health systems deliver care, and emerging trends suggest even more transformative possibilities ahead. Recent research suggests that wearable devices will become more widespread and user-friendly through advancements such as:
- New sensor designs
- Energy-harvesting technologies
- Better integration with clinical workflows
Advanced analytics, fueled by machine learning, will continue unlocking real-time insights that support clinicians in predicting and preventing disease rather than merely reacting to it. Meanwhile, the proliferation of telemedicine and remote monitoring paves the way for more equitable access to healthcare services.
The future of wearables is filled with possibilities, but realizing their full potential requires collaboration. As researchers, clinicians, and industry leaders, we have the opportunity to shape how this technology is used to improve lives. Learn more about collaborating with us to drive progress in computational health innovation.
Amanda Randles, Ph.D., is Director of the Duke Center for Computational and Digital Health Innovation and Alfred Winborne Mordecai and Victoria Stover Mordecai Associate Professor of Biomedical Engineering at the Pratt School of Engineering.